Research has shown that there is a strong link between those diagnosed with coeliac disease and an increased incidence of bone fractures, even for those strictly adhering to a gluten free diet. The increase is higher for coeliac females (1). This is not great news for the 1/60 female Australians out there currently diagnosed with coeliac disease.

What is Osteoporosis?
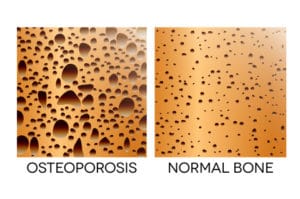
Osteoporosis is a condition where bone density becomes critically low, resulting in thin and fragile bones that have an increased risk of fracturing. It is well known that there is a greater risk of osteoporosis developing for those with coeliac disease, mainly due to the associated malabsorption gut issues inhibiting the absorption of calcium and other essential vitamins (D, K & magnesium), which are the building blocks for our bones. It is also known that the coeliac autoimmune inflammatory response itself produces bone adverse antibodies, responsible for accelerating the breakdown of bone structures in the body. (2)
An added issue is the co-morbid intolerance to dairy products or lactose that many coeliacs face due to the sustained intestinal damage evident even after removing gluten from their diet. This results in the most common source of daily calcium intake, dairy products (milk & cheese & yoghurts), being removed from the diet of many coeliacs, exacerbating a reduced intake of calcium post coeliac diagnosis.
So, should we panic?
Absolutely not. But it is a reminder that we do need to take this health issue seriously, and that we need to be proactively engaging with our doctor to monitor our bone health.
A few years ago I had a bone density scan to do just that. It was shown that I have osteopenia, which is the precursor to osteoporosis. I was at the time already taking calcium supplements, as I was aware of this risk. However I have now also increased my intake of foods naturally containing calcium, such as dairy, and am aware of spreading this intake throughout the day as the body can only absorb about 500mg at once and will flush the rest out. Hopefully when I have a follow up scan it will show an improvement!
The good news is that bone health may be restored with careful monitoring of calcium intake, if instigated early enough, but it can take some time, and regular monitoring is prudent to ensure the remedial measures are being effective.
It is also important to note that the extent of the damage that may have occurred prior to coeliac diagnosis can take a while to turn around, and might influence the recovery rate once remedial measures are applied.
What can you do to prevent yourself becoming one of theses stats?
Request a bone density scan from your doctor to establish your bone health. Thankfully in Australia these scans are freely available to coeliac disease patients at no cost, with a doctors referral.
Ensure you adhere strictly to a gluten free diet to limit ongoing intestinal damage and promote healthy nutrient absorption
Increase your calcium intake throughout your day. Common sources of calcium include dairy (or lactose-free dairy products), broccoli, leafy green vegetables, fish (bones), tofu, almonds & brazil nuts, sesame seeds….
Take calcium supplements if recommended to by your doctor. Choose one which includes vitamin D as it aids in the absorption of the calcium molecules.
Incorporate weight bearing exercise into your daily routine as this increases bone strength
Cut back on salt & caffeine as both may make your body lose more calcium and bone (3)
(1) Adams, Jefferson (2014): Bone Fracture Risk Double for Celiac Disease Patients, celiac.com
(2) Shikhman, A.R. (2012): Risk Factors for Osteoporosis and Coeliac Disease, Journal of Gluten Sensitivity, Institute for Specialised Medicine
(3) Wheeler, Tyler, MD (2018) Osteopenia Treatment, webmd.com
To READ MORE about the impacts of Coeliac Disease you can check out When Gluten Free is NOT Gluten Free or Please Take Coeliac Disease Seriously. Love Us. Coeliacs of the World xx










