We all know one. We all secretly envy them…or, you know, hate them.
The Asymptomatic Coeliac.
They waltz through life NOT having bloating, or tummy cramps, or IBS, or hideous skin rashes.
They just go ‘oops! Oh no, I accidentally ate gluten’.

Whether they feel really really bad about this, or just a little bit bad, or don’t care at all because they just enjoyed hot chips from a shared fryer so life couldn’t be better really…it still does not seem fair and so we (the collective symptomatic coeliac community) feel the need to bring them down a peg or two and let them know, very compassionately of course, that they are still causing internal damage and so, well, the party is over, and Get Responsible!
But really, what the heck is going on here? Why does one coeliac react to traces of gluten with violent cramps, nausea and vomiting, while others get nothing, nada, not even a headache.
What is going on?
Yes, the accepted understanding is that internal damage IS still occurring within those coeliacs who don’t exhibit obvious symptoms to a glutening…their autoimmune system is still in attack mode and launches an offensive against their villi (the nutrient absorption structures within our intestine that supplies all of the essential nutrition to our entire body, via the blood stream), causing the villi to become further damaged (atrophied).
But if their villi are becoming just as damaged as that of symptomatic coeliacs, WHY are they not exhibiting symptoms?? This just does not make sense.
My background as a biology teacher had me asking why?
So lets Science the heck out of this.
(if you can’t be bothered to get all sciencey, just head to the end of the blog for the Takeaways)

Why Are The Symptoms of Coeliac Disease So Different for Different People?
If symptoms are the result of malabsorption of vitamins & nutrients via the in-situ response within the digestive system, which they are (READ MORE about Symptoms HERE), then anyone who triggers the autoimmune response to gluten within their body by ingesting gluten, & subsequently causing damage to the villi in their digestive system, SHOULD exhibit symptoms, because their digestive system will then of course not function properly, causing a lack of essential nutrition (due to malabsorption) to be delivered around their body.
So what is really going on? Why do coeliacs all respond very, very differently to exposure to gluten, and what on earth is the deal with The Asymptomatic Coeliac?
A very thorough report recently published in BMC Medicine (2019) [1] thankfully addressed this exact question (among other things). And the summarised conclusion was, in layman’s terms, not all glutening is equal.
And here is why.
Becoming More Reactive to Gluten
We have all (from what I’ve heard incidentally through social media chat at any rate) had the experience that the longer we have been gluten free, the more ‘reactive’ we have become to gluten exposure. Smaller amounts of gluten exposure start to trigger more intense, or new symptoms.
When I was first diagnosed, 18 years ago now, my immediate symptoms to eating large amounts of gluten (ie a sandwich) was bloating, immediate fatigue, and recurrent mouth ulcers. I also had an intolerance to large amounts of dairy (eg. a milkshake), although I’ve since discovered it is actually only lactose that causes me problems. Generalised symptoms at the time that I had not yet associated with gluten were frequent headaches/migraines, and iron deficiency/fatigue.
However I could eat gluten free food that was cross contaminated without any observable symptoms. So hot chips from a shared fryer with the family happened regularly, I did not need to worry about my meat being cooked on the same grill as gluten-infused meat, and I could tolerate many products with small amounts of gluten such as soy sauce, flavoured chips, dips etc. It really was just obvious wheat based products (breads, flour etc) that caused me problems.
Now however…cross contamination is my enemy. I have to be careful of it all, or I will react. I also have new and wonderful symptoms such as skin rashes, eye issues, nausea, brain fog, and stronger & more frequent headaches & migraines. Fun times.
So why is this happening.
What is going on physiologically?
The Physiology of Coeliac Reactions
At first, prior to diagnosis and shortly after, the body has usually been exposed to a lot of gluten. So while it believes that gluten is not OK (once the coeliac gene has been ‘turned on’), it is thought to only form the offensive when a threshold of gluten ingestion is reached [2]. However, once gluten is removed from the diet, the auto immune system is triggered into response by smaller and smaller amounts of gluten as it more easily identifies it (wrongly of course) as an enemy (now not usually encountered) that needs to be destroyed. Its response is to damage the absorption point (villi) to prevent gluten from being transferred into the blood stream.
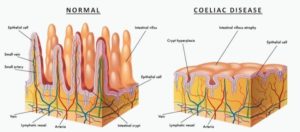
The flow on effect of this, is that many of the other nutrients & vitamins that the body needs to function well, are also prevented from being transferred into the bloodstream, and subsequently transported to areas of need. Thereby causing an element of malnutrition and the inability for the body to function correctly…hence symptoms.
In the BMC Report Coeliac Disease: A Comprehensive Review [1], outlining the latest research and understanding of coeliac disease, the discovery and inherent conclusion was that there IS a different ‘level’ of response by the immune system to gluten within the diagnosed coeliac population. That not all us have the same degree of subsequent damage to villi post gluten exposure, and therefore there will be different degrees of symptoms as a result.
To me, THIS makes so much more sense than the simple idea that “you are also being damaged to the same degree, even though you have no symptoms, so get responsible and strictly avoid gluten like the rest of us”.
The Asymptomatic Coeliac
The report ventured to conclude that those who are asymptomatic are so because they potentially have minor damage to their villi.
Diagnosis may have been made according to a focus on serology (blood test), and only minor villous atrophy (damage to the villi) [1]. Some are diagnosed as having Potential Coeliac Disease (PCD) because they have a positive serology and coeliac genetic markers, but no villous atrophy. Additionally, according to Alessio Fasano, MD, one of the report’s authors, as endoscopic testing only tends to biopsy a small portion of the first section of the large intestine, making conclusions based on this that the entire length of it is damaged is flawed, when in fact the remaining length may still be perfectly healthy. He stated that it was “intuitive that if your damage is only at the beginning and the rest of the intestine is spared, you may be more in the asymptomatic group” [3].
In other words, if the rest of the intestine is in fact still healthy, it would allow for greater overall absorption of essential nutrition, and therefore the body can function quite well, causing no or minor symptoms. This could thus be the reason why some coeliacs have no symptoms when glutened (ie. asymptomatic). There is little initial damage to the villi (ie. only a small section damaged, but enough to result in a positive endoscopic result for coeliac disease), and potentially only minimal or no damage occurring to new gluten exposure (dependent on the extent of gluten exposure).
The report went on to further propose that some asymptomatic coeliacs may actually be misdiagnosed, based on wrong conclusions to very minor damage (below the recognised required level for diagnosis) to the small intestine, as there can be some discrepancies in testing analysis protocol by gastroenterologists world wide. Additionally, as mild villous atrophy can also be caused by non-coeliac related conditions, such as food allergies, parasitic infections, gastroenteritis and Crohns disease, some cases of asymptomatic coeliac patients would require screening for coeliac genetic markers to verify a coeliac diagnosis [1].
There was also the suggestion from one of the studies reviewed in the report that perhaps the PCD asymptomatic coeliac should NOT in fact remove all traces of gluten from their diet, as in doing so they could cause their autoimmune system to become MORE responsive to lower levels of gluten, triggering full blown coeliac responses & damage, which would otherwise have been avoided [1]. In one study, only 6% of asymptomatic coeliacs who returned to a gluten containing diet developed villous atrophy [4]. This is clearly quite a controversial scientific position to take, according to current coeliac guideline norms, and further research would be required to substantiate this hypothesis.
Impact of Later Life Coeliac Diagnosis
In line with other scientific studies however, the report also proposed that coeliacs diagnosed later in life (over 50 years of age), may continue to exhibit digestive symptoms & have persistent villous atrophy even after adhering to a strict GFD [1]. This is often identified as either Refractory Coeliac Disease (RCD), occurring in less than 5% of coeliacs, or ongoing active coeliac disease (OACD)[1,5]. Additionally such patients can have an increased chance of developing the more life threatening symptoms such as bowel cancer and osteoporosis [1]. This is potentially because the impact of consuming gluten for the added length of time prior to diagnosis, has increased the overall effect of nutrient malabsorption on the body [1]. It could also be suggested that the intestine had by then accumulated so much damage that a strict gluten free diet would not be sufficient to fully restore complete healing of the villi and subsequent efficient nutrient absorption, accounting for the ongoing digestive symptoms [6,7].
While I have not been diagnosed with RCD or OACD, I do place myself in this generalised category of later in life diagnoses (at age 37) causing ongoing malabsorption issues despite a strict adherence to a GFD (with bloods and follow up biopsies confirm a normalised gut). I am faced with almost a trailer load of vitamin supplements to take each morning to subsidise what my body is still not absorbing naturally from my food (Vit B12, l-lysine, calcium & Vitamin D…). I also have osteopenia, which is unlikely to be reversed. However, through calcium supplements it is hoped it will not develop into full-blown osteoporosis. You can READ MORE about Coeliac Disease and the link to OSTEOPOROSIS HERE.
So what are the takeaways here?
There is a wide variety of responses by coeliacs to exposure to gluten (types & severity of symptoms).
Those who seem to exhibit no obvious symptoms are deemed Asymptomatic
The asymptomatic coeliac may actually be exhibiting non digestive related symptoms that they have not yet linked to their disease (eg. headaches, muscle soreness, skin conditions, brain fog, anxiety, miscarriages etc).
Asymptomatic (& PCD) coeliacs may be experiencing no symptoms because they have less damage to their villi and/or their auto immune system is not as responsive to gluten exposure as other coeliacs, therefore causing less or no damage to their digestive system (villi) with trace exposure to gluten, and no obvious digestive symptoms.
Diagnosis later in life may have caused irreversible damage to some villi of the digestive system, resulting in some ongoing symptoms despite adherence to a strict gluten free diet, and an increased risk in the development of non-digestive coeliac associated malignant diseases
Some asymptomatic coeliacs may actually be wrongly misdiagnosed (ie. not coeliac) due to discrepancies in world wide coeliac diagnostic testing protocol.
Gluten sensitivity by the auto immune system (& symptomatic response) can increase after an individual removes gluten from their diet.
While all of these thoughts on how coeliac disease can manifest so differently DO make scientific sense to me, and were presented by a collaboration of well respected scientists, some of the statements are based on quite controversial hypotheses yet to be confirmed by further scientific study. So, current advice from gastroenterologists and local Coeliac Societies should still of course be adhered to.
And the bottom line:
All diagnosed coeliacs should adhere to a strict gluten free diet for life and avoid cross contamination where possible.

In conclusion however, it is clear that not all glutening is equal.
We cannot use a cookie cutter approach to interpreting the effect of the disease on a person’s body, or how an individual should manage their diagnosis. The asymptomatic coeliac may have little or no villi damage from new exposure to small amounts of gluten, or they may still be causing incremental damage that will accelerate over time, resulting in symptoms becoming obvious and eventually more significant to their health. They should of course still avoid gluten, but it is definitely probable that they simply do not have the same auto immune response & subsequent villi damage to traces of gluten that the highly symptomatic coeliac does.
Not all glutening is equal.
We are very thankful for this comprehensive report [1], and for the research that continues world wide, including the ground breaking research from our own Australian team at the Walter & Eliza Hall Institute of Medical Research, headed up by Dr Jason Tye-Din. It is wonderful that the looking glass into this disease is getting clearer and clearer, giving us a more accurate picture of what is going on within our bodies. Hopefully their understanding and discoveries will one day lead scientists to either finally find a cure, or at least better & less impactful ways to manage our disease.
What are your thoughts and experiences?
LOVE ![]() you to share them in the COMMENTS below.
you to share them in the COMMENTS below.
For MORE INFO on Coeliac Disease you can head to these other BLOGS:
Does A Coeliac Diagnosis Mean That Life Has to Stop?
Are Our Bones at Risk? What All Coeliacs Need to Know About Osteoporosis
Cross-Contamination: When Gluten Free is NOT Gluten Free
Free Downloadable: Coeliac Safe Food Handling Practices
Or contact your local Coeliac Society.
[1] Caio G, Volta U, Sapone A, Leffler A L.,De Giorgio R, Catassi C, Fasano A. Celiac disease: a comprehensive current review (2019), BMC Medicine.
[2] Fazekas de St Groth, B. Prof of Immunolgy, Centenary Institute. How clean is too clean? Trust your gut instincts (2011) www.thecoversation/healthandmedicine.com. Accessed 25.1.20
[3] Cohen S. Asymptomatic Disease (2018), Gluten Free Living Magazine
[4] Voita U, Caio G, Giancola F, et al. Features and progression of potential celiac disease in adults. Clin Gatroenterol Hepatol. 2016;14;686-93.
[5] Tye-Din J. When the gluten free diet stops working: refractory coeliac disease (2012), Australian Coeliac Magazine
[6] Treatment of celiac disease. The University of Chicago: Treatment Disease Centre. www.cureceliacdisease.org. Accessed 25.1.20
[7] Lanzine A, Lanzarotto F, Villanacci V, Mora A, Bertolazzi S, Turini D, Carella G, Malagoli A, Ferrante G, Cesana BM, Ricci C. Complete recovery of intestinal mucosa occurs very rarely in adult coeliac patients despite adherence to gluten free diet (abstract). 2009. US National Library of Medicine. www.ncbi.nlm.nih.gov.com. Accessed 25.1.20








I’ve just read your article in the coeliac magazine and I had to comment.
As a mum of 2 kids with coeliac disease with severe symptoms, the article evoked some very strong emotions from my eldest daughter and myself.
I suppose by your definition we are ‘coeliac extremists’. My eldest daughter has developed a great deal of anxiety around food due to her condition, and we have very limited options where we can eat. It puts huge amounts of pressure on me as a mum. I used to love baking but catering for my kids dietary requirements over the past 8 years has drained the joy out of food prep… and yet I have to continue because there are next to no other options.
One of the most frustrating issues for us is that food vendors do not understand the importance of 100% gluten free requirements for coeliacs. This is compiled when (as I’ve personality experienced) other coeliacs say, “oh it’s fine that there was a contaminant in the fryer, that won’t affect me”, which reinforces the idea that we are…. ‘extremists’ when in fact, we are just doing what the condition requires. If you receive unkind or unsolicited advice about your condition that is unfortunate, and I’m sorry some people are rude. But if you advocate for people with coeliac to choose their own risk assessment it actually has a very negative effect on the already uphill battle that we ‘extremists’ face to try and get our needs met so we can recover our mental health too.
I agree with you let’s be kind to each other, maybe start by not labeling us with derogatory names that really just define the medical advice for managing coeliac disease.
Hi Emma, so sorry to hear about the struggles your daughter has staying healthy, and your difficult journey to keep her food safe. I do not label anyone a ‘coeliac extremist’ simply because they have to be super vigilant to prevent cross contamination, and I apologise if my article read that way. My point about the so called ‘extremists’ is when they force their requirements on every other coeliac in an unkind, ungracious and judgemental way. I would definitely assume that was not your stance. I also understand that some who approach CC from a more relaxed attitude because they are either not coeliacs or minor CC does not affect them, it can cause some confusion in the food catering industry. However I do believe they still should have the freedom to eat the way they can, and the rest of us who have to be more careful just have to keep asking the right questions and sharing the intel about the venues that do understand good CC prep/handling. I wish you and your daughter many many amazing coeliac safe food moments together 🙂 Jane x
Hi,
I was diagnosed with Coeliac at the age of 47, and went on a GF strict diet for 2 years. I have no symptoms and my villi are fine. I am still on a GF diet and all my blood tests are negative for coeliac. However 2 years ago I ha$ a biopsy and it seems that my duodenum has been affected. My only symptoms are, tiredness, aches and brain fog. I also have Hashimoto’s , NAFLD and fibromyalgia . I guess my question is, how strict should my diet be.
Hi Lidia , so sorry for not replying sooner…my blog has been somewhat neglected for the last couple of years due to the busyness of my GF hamper business. But am happy to be able to get back into it now:)
Your history is very interesting, with other complex health issues definitely making it hard to determine what is causing what. I’m a little confused as to how it has played out for you, but I think you are saying that when you were diagnosed as a coeliac your intestine (villi) cleared up after 2 years of a strict Gf diet, but now it shows damage again (despite your bloods have not indicating antibodies)?
I obviously cannot give medical advice and don’t have full clarity on what your situation is, but I would definitely recommend staying on a strict Gf diet as the coeliac auto-immune reaction to gluten continues for life (until a cure!). The symptoms you mention are definitely in line with coeliac disease, but also can be linked to menopause and potentially your other health issues. Easy to rule out gluten though if you stay clear of it 🙂
Hi Jane, great read, thanks.
I’m an asymptomatic coeliac, diagnosed 12 months ago. I was diagnosed following an iron infusion as my blood ferritin was undetectable, but I had no other symptoms.
The damage to my vili though was extreme and highly visible to the gastroenterologist during my gastroscopy.
So who knows?!
I find it dangerous being asymptomatic as I have NO IDEA if I accidentally ingest gluten, despite my blood tests showing I’m definitely still being exposed.
It’s a wild ride.
Hi Jess, yes our bodies are so complex and there is still so much that scientists have not figured out. The difference in symptoms and reactivity is so broad! I know a couple of asymptomatic coeliacs and they too find it hard to know when they have been affected by CC…and to not be tempted to ‘cheat’! There might of course BE some symptoms, but they haven’t been linked to coeliac disease in your head (or the doctor’s yet) because they are general health issues that may have been put down to something else. That is quite common as well. Definitely a complicated health journey for most of us!
Hi,
Yours is the first article I have read to give me hope. I have an interesting gluten free journey some of which your article has helped me to understand. I’m 51 born in 1969 and lived in Scotland my whole life. When I was small child (long before I can remember) I had issues with failure to thrive, being underweight and malnourished to the point of my parents being suspected of neglect. This wasn’t the case as I had 4 healthy older siblings, 2 years between us all. I was taken in to hospital for a period of time and underwent a whole range of tests, which tests I don’t know, and I have no memory of this period. My oldest sister tells me I was a tiny thing when I went in to hospital and the next time she visited me there, I was crawling and running around, so it must have lasted a while. What I do know is that my parents were told I had Coeliac Disease and so began my G.F life. I followed a strict G.F diet and I have clear memories of this. My mother frightened the life out of me telling me I would be violently ill if I ate gluten. Understandably I avoided it assiduously.
This lasted until I was 16 years old and I decided I would be rebellious and eat the odd regular cake and piece of bread. I had no adverse symptoms and so what started as a few regular cakes turned in to eating anything I liked . Again there were no adverse effects. Quite the contrary, I was 6’2, went to the gym regularly, had a perfect BMI, ran regular 10K races etc. I wasn’t quite an athlete but I was very healthy and have rarely had a day sick in my life. The only thing that happened was a mild onset of guttate psoriasis. the psoriasis over the years became a little worse but not unbearable and so life continued, I didn’t have any coeliac symptoms, no underdevelopment, malnourishment, deficiency or sickness.
Getting fed up with the psoriasis in 2005 or thereabouts when I was around 35 years old I learned about dermatitis herpetiformis. So, I asked to be referred to a dermatologist. I told them my Coeliac story and as opposed to carrying out a skin biopsy for dermatitis herpetiformis, they carried out a blood test for Coeliac disease. At the time I asked didn’t I require an endoscopic biopsy, only to be told that things had moved on and it only required a blood test. I was told the blood tests returned a negative result and that I did not have Coeliac, I asked how that could be as I was positively misdiagnosed as a child. They said, it must have been a mistake and they were sure I was negative for coeliac. I continued to eat a normal diet including gluten . The psoriasis didn’t go away, and I continued with no other symptoms from eating gluten. I literally continued eating whatever I liked.
Fast forward another 13 years, I was 48 years old and was at my local GP to have the winter flu vaccination as part of routine vaccination due to working with vulnerable people in social care. I walked in and the Doc says, “oh I take it this vaccination is because of your selective IGA deficiency?” I said, “my what?”. There and then I learn that I have selective IGA deficiency which was diagnosed when I was a very small child, around the same time as my Coeliac diagnosis. I asked the Doc what this meant. She said it depends how severe my IGA deficiency is, but that I may require to wear a medical alert. She duly conducted a blood test, sent it for analysis and told me the results indicated it was not severe, that I should do nothing and that there was nothing to worry about.
Fast forward another 2 years and almost on my 50th birthday in Nov 2019 I had blood in bowel movements. I had a sigmoidoscopy in March 2020 and they identified inflammation of the mucosa and took some small biopsies. They said the tests showed nothing sinister and this was within the normal range. I had no more blood and felt fine. Fast forward another year to my 5ist birthday. I began to have a range of GI symptoms, some neuropathic type pain and kidney type pain in my left flank. I had a really noisy, crampy stomach but normal bowel movements. I had stool sample tests and urine tests both of which were normal. I had an ultrasound and the report read, “Normal ultrasound appearance of the liver, gallbladder & biliary tree. CBD measures 0.cm. The head & body of the pancreas appears normal; tail is obscured. Spleen is normal in size. Normal right kidney. The left kidney appears unremarkable asides a 1.1cm thin walled cyst which contains a 0.4cm area of calcification within It’s wall. This should be followed up by an ultrasound initially in 3 months time. Normal calibre abdominal aorta. The urinary bladder outlines normally, prostate measures 3.6 x 5.4 x 3.4 cm. No abdominal free fluid.” So all seems normal other than small kidney cyst which they said should not be posing any problems. I also had the following blood tests;
Full blood count
Erythrocyte sedimentation rate
Amylase test
Bone profile
C-reactive protein
Liver function test
Urea and electrolyte test
All of these came back normal, in fact the doc said some of them were in the excellent range. But I still had GI symptoms and left flank pain. I saw a specialist gastroenterologist who told me my negative coeliac blood test in 2005 could have been a false negative due to having selective IGA, and that my symptoms could be gluten related. So I began to look in to it further. I began to learn more about Coeliac than I have ever known but left terrified that 35 years of gluten may have caused villous atrophy, renal damage, peripheral neuropathy or worse! So, this article has given me some faith that I may not have completely destroyed my body. The Gastroenterologist is going to review my historic records and try to make some sense of my history before he decides what to do next. in the meantime, I’ve decided to go gluten free and 1 week in after some worsening GI symptoms, things have settled down. I still have the left flank pain and some weird neuropathic symptoms. So, lets see what happens next.
Oh goodness, what a frustrating journey you have been on. Getting inaccurate diagnoses can be a common problem, but I’m glad you now finally have some answers. I hope further clarity is found with a potential re-confirmation of coeliac disease, and ongoing avoidance of gluten leading to a decrease in your continuing health issues. The body is a very complex one, and the fact that there is such a wide variety of the clinical presentations of the ‘switched on’ coeliac gene aids in misinformation and incorrect diagnoses in many instances. Hopefully science continues to bring us more clarity! Thanks so much for sharing your story. Jane x